You may have noticed that gift gifting was a bit more difficult this holiday season. Those two mighty standbys for the gift-givers, perfume, and neckties, have moved from the ‘always welcome’ list to the ‘What was he or she thinking?’ list.
Perfume – oh, that never-surprising but always-delighting gift – isn’t the gift it used to be. The problem is scent wearing by women has fallen off, as health concerns about volatiles in the air have grown and casual dressing, especially in the time of pandemic, is de rigeur.
Pity – luxury perfume was the unchallengeable gift. It was giving on the strength of its brand, like Miss Dior or Chanel No. 5. Labels really counted in fragrance giving. You were ill-advised to try anything out of the usual. If you espied something called, say, Rocky Mountain Rose, you were advised to eschew it.
The best and easiest to give was Joy by Jean Patou. The fragrance advertised itself as “the most expensive perfume in the world.” Bingo! You couldn’t go wrong if you had the bucks. I used to give a small bottle of Joy to my office manager every year and was thanked with oohs and aahs, even though she knew what was coming. She explained that a woman’s real use of Joy wasn’t so much in wearing it (and she wore it with pleasure), but in displaying it – showing her friends how much her significant other loved her. I rush to say that wasn’t my role in her life.
Neckties were the perfect gift for the man who might have everything. A man couldn’t have too many, and a new one in the style of the day was genuinely welcomed to the sartorial collection.
The necktie is rapidly going the way of spats, detachable collars, and Homburgs, to oblivion.
So shed a tear for the necktie and its infinite giveability. You could play the brand game, but there was no need for that. An obscure neckwear maker, doing a good job with the silk or wool, would be just as fine an accoutrement, as a luxury name like Givenchy or Ralph Lauren. The outstanding exception to this rule was some fabulous work of art by Liberty of London. That would earn deep approval, a friendship cementer.
As a generalization though, an unknown name in neckwear was just as good as the names of the great designers. To those in the know, the best place to buy ties at a reasonable price is, for reasons unknown, at hotel gift shops. Good ties at great prices.
Ties were in their day so important that good restaurants and clubs had selections of ties to fix up men who came with – Shock! Horror! — an open-necked shirt. The proprietor of a famous Manhattan restaurant of yore, La Cote Basque, told me he wouldn’t serve a king if he wasn’t wearing a tie. La Cote Basque has long gone and so that poor man was never put to the test of facing down royalty.
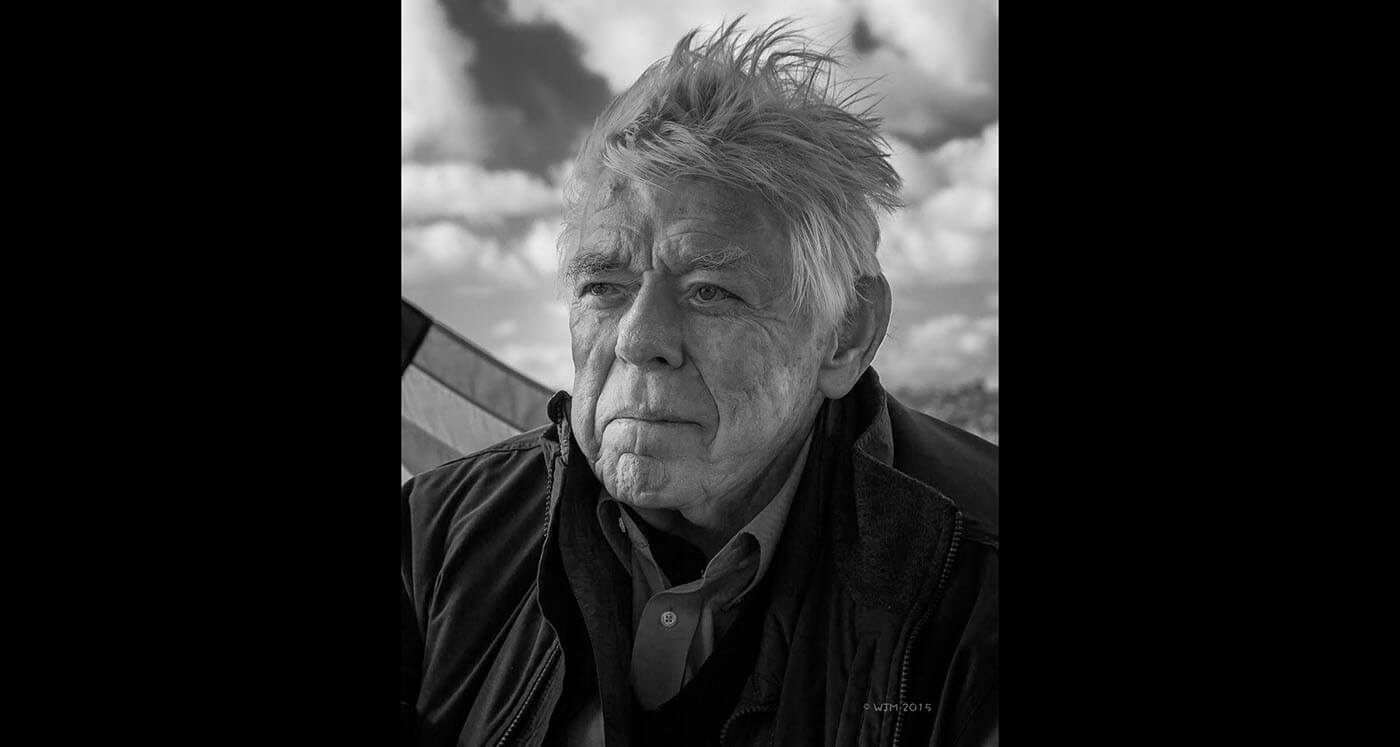
I wear a bowtie. I have Tucker Carlson – yes, that Tucker Carlson — to thank for that change in my appearance, that bit of sartorial shtick. When I met Carlson, long before he found, as one writer said of someone else, the cramped space to the right of Rupert Murdoch, he was a funny, likable conservative who had just left a CNN talk show and authored an amusing book about the experience of being TV chatterer.
I had him as a guest on my television program, “White House Chronicle” on PBS. He was known as a bowtie-wearer and, as a joke, I donned one. I got so many favorable comments that I’ve taken to wearing them instead of the long, silk emblems of the once well-dressed man.
Shame, I say, on the retreat of perfume and the near extinction of the necktie. Women don’t smell so elegant, and men look unfinished.